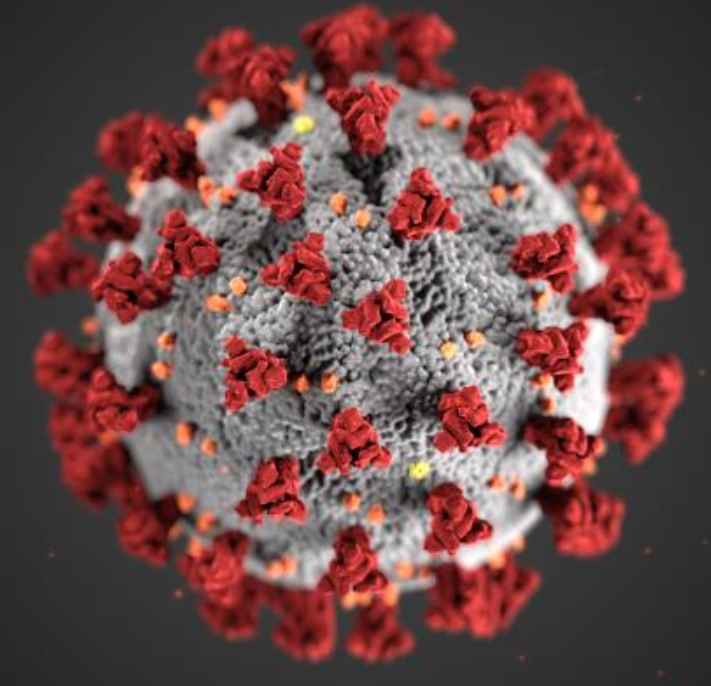
COVID-19 (coronavirus disease 2019) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). First detected in 2019 and declared as a pandemic in 2020, COVID-19 has greatly affected the lives of people across the globe and will continue to do so for many years to come. Like other public health emergencies, the impact of the pandemic on the health and wellbeing of women is unique and, in some cases, particularly severe. In addition to sex-mediated differences in women’s experience of COVID-19 infection, research has associated the pandemic with gendered inequalities in health care access and outcomes,i increased violence against women and girls,ii and heightened anxiety and depression in women.iii Women are disproportionally affected by Long COVID.iv The pandemic also significantly disrupted the careers of women, particularly those with childcare or caregiving responsibilities.v With a better understanding of the unique impact of this pandemic on the health and careers of women, we can better prepare for, and mitigate the impact of, future public health emergencies.
The COVID-19 pandemic underscored the imperative of systematically considering biological and social determinants of health to strengthen our collective capacity to respond equitably to the health crisis—as well as to future health crises. Sex (as a biological variable) and gender (as a social and structural variable) influence health and disease as independent and interactive factors. Understanding the influences of these variables in disease prevalence, progression, treatment response, and health outcomes is critical to addressing and preventing health disparities.
COVID-19 research that accounted for sex, gender, and other key variables (e.g., race, ethnicity, age) enabled the development and deployment of vaccines, diagnostics, treatments, and interventions that are relevant to and effective for the entire population. Below are a few areas of scientific inquiry related to COVID-19 in which the consideration of sex and gender deepened our understanding of the disease and associated public health issues.
Mental Health: The pandemic demonstrated an anxiety gap between men and women, with women being more likely to report anxiety during the pandemic.vi During the pandemic, the use of alcohol exceeding the recommended daily limits was greater for women than for men.vii
Intimate Partner Violence: Data indicated an increased risk of intimate partner violence (IPV) during the pandemic for women.viii Limited access to health care services, including IPV support services increased the difficulty of identifying, reporting, and responding to IPV.
Pregnancy, Breastfeeding, and Reproductive Health: Pregnancy is associated with alterations in the immune system, and pregnant women are more susceptible to respiratory pathogens and to the development of severe pneumonia than the general population. Pregnant women who have COVID-19, especially if they have chronic diseases or maternal complications, may have higher risks of complications if hospitalized for their COVID-19 episode.ix
COVID-19 Vaccinations and Menstrual Cycles: The administration of COVID-19 vaccines has been studied in relation to possible menstrual cycle irregularities. In an NIH-funded study of 4,000 individuals, the average menstrual cycle change is less than 1 day in the cycle in which the vaccine was administered. The study found no changes to the length of menstrual flow. The change in the length of the menstrual cycle may be related to the phase of the menstrual cycle in which the vaccine was administered, with the only change in the menstrual cycle length found in individuals who had the vaccine dose in the first half of the menstrual cycle.x
Sexual and Gender Minorities: Prior to COVID-19, research had shown that sexual and gender minority (SGM) populations experienced unique health disparities, including poorer health-related quality of life; greater risk of suicide; increased risk of mistreatment, discrimination, and violence; increased risk of post-traumatic stress disorder; and increased exposure to other stresses and stigmas associated with negative clinical effects. Further health and health-related disparities exist for SGM individuals from racial and ethnic minority groups, and some SGM subpopulations have an increased risk of diabetes, fatal violence, unemployment, and/or additional stress and stigma. The COVID-19 pandemic exacerbated health disparities for SGM populations.xi
Long COVID: Long COVID, long-haul COVID, post-COVID-19 condition, chronic COVID, and post-acute sequelae of SARS-CoV-2 (PASC) are all names for the health problems that some people experience 3 or more months after a COVID-19 diagnosis.xii Approximately 7-11% of adults who have had COVID-19 infections experience Long COVID.xiii Women are more likely to experience Long COVID, with women representing up to 60-80% of the total proportion of individuals with this diagnosis in some studies.xiv Long COVID symptoms are large in number, with up to 200 symptoms associated with this umbrella diagnosis, including muscle and joint aches and pains, as well as respiratory, nervous, mental health, cardiovascular, and gastrointestinal symptoms. Women may experience different symptoms of Long COVID compared to men, including possible changes to menstrual cycles. ORWH is participating in the government-wide effort to better understand this health condition and participates in the HHS Long COVID Task Force.
The pandemic also greatly impacted the careers of women, including those in science, technology, engineering, mathematics, and medicine (STEMM) fields.xv As the majority of health care providers are women, women in health care professions shouldered enormous mental and physical strain to meet the increased burden of the pandemic while caring for many critically ill patients. Many women were challenged further by their domestic roles as principal caregivers. With many schools and day care centers closed and education systems adopting at-home virtual learning models, a disproportionate number of women shouldered increased responsibilities for childcare, home-schooling, and managing their children’s psychological responses to COVID-19—all while navigating their own pandemic-related stress, hardships, and health issues.
Published in 2021, the NIH-supported National Academies of Sciences, Engineering, and Medicine (NASEM) book-length report, The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine, details the pandemic’s disruption of the professional development of women in STEMM fields. The publication describes how lockdowns and mitigation efforts disrupted global scientific conferences, laboratory research, work routines, and virtually every aspect of professional activity. Initial research and evidence cited in the report indicate that COVID-19 had particularly adverse effects on the engagement, experience, and retention of women in STEMM, and may have resulted in the loss of some pre-pandemic achievement gains made by women in academic science. The NASEM report also speculates about the influence of these disruptions on the careers of women in STEMM, both positively and negatively, in future years.
ORWH was actively engaged during the pandemic response and supported mission-critical NIH efforts in an array of different ways, including:
- Development of ORWH’s strategic approach to the COVID-19 response
- Launch of the first iteration of the Women, Science, and the Impact of COVID-19 webpage
- Launch of the COVID-19 and Maternal Health webpage
- Expansion of the scope of ORWH’s funding announcements to include COVID-19-related research, such as through the ORWH Sex and Gender (SAGE) Administrative Supplement Program and Understudied, Underrepresented, and Underreported (U3) Administrative Supplement Program
- Participation in many NIH COVID-19-related funding announcements
- Publication of funding mechanisms to support women in Science, Technology, Engineering, Mathematics, and Medicine (STEMM), including several co-funding applications to support researchers providing care for family members with COVID-19
- Development of Guiding Principles: Sex and gender influences in COVID-19 and the health of women and a COVID-19 Digest: Resources and Consideration for Sex, Gender and COVID-19 Research
- Launch of a Webinar Series, “Diverse Voices: Intersectionality and the Health of Women”
- Participation in various NIH initiatives and activities such as the Rapid Acceleration of Diagnostics (RADx); the Community Engagement Alliance Against COVID-19 Disparities (CEAL); the NIH Pediatric Research Consortium’s (N-PeRC) Maternal Child Health subgroup; Digital Health; and Research, Condition, and Disease Categorization (RCDC) System
- Participation in the National Vaccine Advisory Committee
- Addition of the women’s health perspective to the NIH-wide Strategic Plan for COVID-19 Research (Priority 4 & 5)
- Establishment of an NIH-wide Coordinating Committee for Research on Women’s Health (CCRWH) COVID-19 Working Group, co-chaired by Drs. Rajeev Agarwal, Marrah Lachowicz-Scroggins, and Nina Schor
- Performance of many activities under the umbrella of the CCRWH COVID-19 Working Group such as portfolio analysis and publication of a Request for Information
- Publication of articles in peer-reviewed journals
- Publication and promotion of a Director’s Message blog focused on COVID-19 and women online and on social media platforms
Disclaimer: The citations on this page, in the guiding principles document, and in the annotated bibliography constitute neither an endorsement by ORWH or NIH nor an indication that these references have been peer-reviewed or NIH-funded.
i Flor, L. S., Friedman, J., Spencer, C. N., Cagney, J., Arrieta, A., Herbert, M. E., Stein, C., Mullany, E. C., Hon, J., Patwardhan, V., Barber, R. M., Collins, J. K., Hay, S. I., Lim, S .S., Lozano, R., Mokdad, A. H., Murray, C. J. L., Reiner, R. C. Jr, Sorensen, R. J. D., Haakenstad, A., Pigott, D. M., & Gakidou, E. (2022). Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: A comprehensive review of data from March, 2020, to September, 2021. Lancet, 399(10344), 2381–2397. https://doi.org/10.1016/S0140-6736(22)00008-3
ii Burki, T. (2020). The indirect impact of COVID-19 on women. The Lancet Infectious Diseases, 20(8), 904–905. https://doi.org/10.1016/S1473-3099(20)30568-5
Fogstad, H., Langlois, E. V., & Dey T. (2021). Covid-19 and violence against women and children: Time to mitigate the shadow pandemic. BMJ, 375, n2903. http://doi.org/10.1136/bmj.n2903
iii Kupcova, I., Danisovic, L., Klein, M., & Harsanyi, S. (2023). Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychology, 11(1), 108. https://doi.org/10.1186/s40359-023-01130-5
iv Fang, Z., Ahrnsbrak, R., & Rekito A. (2024). Evidence mounts that about 7% of US adults have had Long COVID. JAMA, 332(1), 5–6. https://jamanetwork.com/journals/jama/article-abstract/2819957ht
v National Academies of Sciences, Engineering, and Medicine. 2021. The impact of COVID-19 on the careers of women in academic sciences, engineering, and medicine. The National Academies Press. https://doi.org/10.17226/26061
vi See note 3.
vii Barbosa, C., Cowell, A. J., & Dowd, W. N. (2021). Alcohol consumption in response to the COVID-19 pandemic in the United States. Journal of Addiction Medicine, 15(4), 341–344. http://doi.org/10.1097/ADM.0000000000000767
viii See note 2.
ix Matsuo, K., Green, J. M., Herrman, S. A., Mandelbaum, R. S., & Ouzounian, J. G. (2023). Severe maternal morbidity and mortality of pregnant patients with COVID-19 Infection during the early pandemic period in the US. JAMA Network Open, 6(4), Article e237149. http://doi.org/10.1001/jamanetworkopen.2023.7149
Metz, T. D., Clifton, R. G., Hughes BL, et al. (2022). Association of SARS-CoV-2 infection with serious maternal morbidity and mortality from obstetric complications. JAMA, 327(8), 748–759. http://doi.org/10.1001/jama.2022.1190
x Edelman A., Boniface, E. R., Male, V., Cameron, S. T., Benhar, E. Han, L., Matteson, K. A., Van Lamsweerde, A., Pearson, J. T., & Darney, B. G. (2022). Association between menstrual cycle length and COVID-19 vaccination: A global cohort. BMJMedicine. https://doi.org/10.1136/bmjmed-2022-000297
xi Pharr, J. R., Terry, E., Wade, A., Haboush-Deloye, A., Marquez, E., & Nevada Minority Health And Equity Coalition. (2022). Impact of COVID-19 on sexual and gender minority communities: Focus group discussions. International Journal of Environmental Research and Public Health, 20(1), 50. http://doi.org/10.3390/ijerph20010050
Brewer, K., Mantey, D. S., Thomas, P. B., Room, K. F., Kong, A. Y., & Alexander, A. C. (2023). Identifying disparities in suicidal thoughts and behaviors among US adolescents during the COVID-19 pandemic. Preventive Medicine, 177, 107791. http://doi.org/10.1016/j.ypmed.2023.107791
Kamal, K., Li, J. J., Hahm, H.C., & Liu, C. H. (2021). Psychiatric impacts of the COVID-19 global pandemic on U.S. sexual and gender minority young adults. Psychiatry Research, 299, 113855. https://doi.org/10.1016/j.psychres.2021.113855
xii National Academies of Sciences, Engineering, and Medicine. (2024). A Long COVID definition: A chronic, systemic disease state with profound consequences. The National Academies Press. https://doi.org/10.17226/27768
xiii See note 9.
xiv See notes 10 and 11.
xv Doyle, J. M., Morone, N. E., Proulx, C. N., Althouse, A. D., Rubio, D. M., Thakar, M. S., Murrell, A. J., & White, G. E. (2012). The impact of the COVID-19 pandemic on underrepresented early-career PhD and physician scientists. Journal of Clinical and Translational Science, 145(1), Article e174. https://doi.org/10.1017/cts.2021.851