Social Determinants of Health: Like Water to a Fish
By Dr. Janine A. Clayton
 As everyone knows, fish live in water—with all its oxygen, nutrients, predators, and pollutants. That’s the environment in which fish thrive or languish. It affects their physiology, behavior, and survival. Similarly, society is our water, and the social determinants of health (SDOH) have a pervasive influence on us and our health—for good and bad, just as with fish.
As everyone knows, fish live in water—with all its oxygen, nutrients, predators, and pollutants. That’s the environment in which fish thrive or languish. It affects their physiology, behavior, and survival. Similarly, society is our water, and the social determinants of health (SDOH) have a pervasive influence on us and our health—for good and bad, just as with fish.
What are SDOH? They are “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.” Globally, SDOH are strongly associated with a wide range of health outcomes and risks, functioning, and quality-of-life. In fact, SDOH are major drivers of health inequities experienced by people across the world.1,2
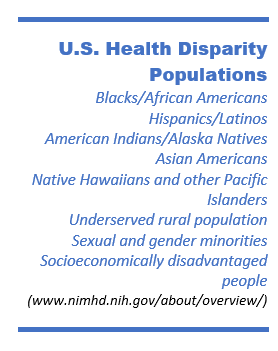
In the United States, various populations experience significant health disparities in one or more diseases or conditions, including hypertension, obesity, cardiovascular disease, cancer, diabetes, and HIV/AIDS.
Crucially, society—through policies, programs, and the purposeful allocation of resources—can moderate these factors.3,4 Researchers call them social determinants, but we should think of them as correlates whose influences may be malleable to intervention. However, society must act on the results of SDOH research to improve health for everyone.5,6,4
- Locations with high levels of resources and status are strongly linked to good health—from reduced risk factors for and rates of chronic diseases to lower mortality from the leading causes of death, and, ultimately, longer lives.9,10 On the other hand, physical environments with poorer air and water quality are linked to socioeconomic disadvantages.11
- Environments with multiple grocery stores well stocked with nutritious food, extensive public transportation, safe places to walk, and green spaces for exercise and leisure promote healthy behaviors, such as diet and exercise.12,13
- Place is also associated with access to high-quality education and job opportunities, affordable housing, low crime rates, and availability of social capital and support.12,7
- Location contributes to sense of security and well-being, level of social participation, and likelihood of experiencing discrimination and incarceration.7,6
- Finally, place is also associated with access to and the affordability and quality of clinical care as a consequence of available employment with health insurance, low-cost transportation options (e.g., mass transit) for appointments, nearby hospitals, and medical practices.8,7,14,15
Many health organizations are increasingly addressing the broader conditions that people experience.6,16,17,4 Because health care providers interact with diverse patients and already talk with them about factors affecting health and wellbeing, they are particularly well positioned to address SDOH. Provider reimbursement, health care administration, and physician training must change to enable providers to incorporate SDOH into care. For example, practices can integrate small-scale social care—by being aware of factors such as limited access to transportation and adjusting with tele-health provision, assisting with vouchers, or advocating at the community level.18 Similarly, biomedical researchers can help address SDOH by incorporating them into their studies.
Through a willingness to incorporate SDOH in our work, we can leverage a growing base of evidence and practice to ensure that the “water” all around us—the places where we live, learn, work, and play—not only promotes our health but helps us thrive.
Place, Race, and Health
Factors that contribute to health, health care, and overall health and life expectancy are spatially patterned by ZIP code and Census tract in the United States.19 Another, more specific factor related to ZIP code and Census tract—residential racial isolation of Black people—is a particularly strong predictor of a wide range of negative health outcomes, such as infant and adult mortality, type 2 diabetes, hypertension, and poor maternal and cardiovascular health.5 Geographic patterns of residential racial isolation appear to have historical roots and overlap with contemporary factors, including lower educational attainment. Between 1990 and 2015, 30 percent of Census tracts grew more racially isolated and 14 percent, less isolated; 57 percent remained stable.5 Researchers can map residential racial isolation and its associations with health outcomes and other SDOH to understand health disparities and how to intervene to reduce them.5 This powerful tool allows investigators to study policy drivers retrospectively and predict health outcomes prospectively.5
References
1 World Health Organization. Social determinants of health. https://www.who.int/social_determinants/sdh_definition/en/ (accessed August 4, 2020).
2 Health equity refers to a principle of social justice (i.e., every person, including those in economically/socially disadvantaged populations, has the possibility to be healthy); health disparity is a metric for measuring progress toward health equity. Braveman, P. Public Health Rep. 2014. PMID: 24385658
3 Singh, G. K., et al. Int J MCH AIDS. 2017. PMID: 29367890; PMCID: PMC5777389.
4 Robert Wood Johnson Foundation Commission to Build a Healthier America. Beyond health care: New directions to a healthier America. 2009. http://www.commissiononhealth.org/Recommendations.aspx (accessed August 5, 2020).
5 Miranda, M. L. Assessing residential segregation’s role in shaping health and wellbeing. Presentation at ORWH U3 Program’s Women’s Health Lecture Series: Improving Chronic Disease Outcomes Through Approaches that Address Social Determinants of Health. https://www.youtube.com/watch?v=hDr4s45e0Yw&feature=youtu.b
6 Artiga, S., & Hinton, E. Beyond health care: The role of social determinants in promoting health and health equity. Kaiser Family Foundation Issue Brief, May 2018. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ (accessed August 4, 2020).
7 Healthy People 2030. Social determinants of health. Available from https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed August 18, 2020).
8 Gornick, M. Disparities in health care: Methods for studying the effects of race, ethnicity, and SES on access, use, and quality of health care. Institute of Medicine. 2002. https://pdfs.semanticscholar.org/19c1/98d00ed6e66d646d6650ea20e4d0b8eb63b1.pdf (accessed August 20, 2020).
9 Singh, G. K., et al. Int J MCH AIDS, 2017. PMID: 29367890; PMCID: PMC5777389.
10 Braveman, P., & Gottlieb, L. Public Health Rep, 129 Suppl 2. 2014. PMID: 24385661.
11 Forno, E., & Celedon, J. C. Curr Opin Allergy Clin Immunol. 2009. PMID: 19326508.
12 Robert Wood Johnson Foundation. Built Environment and Health. https://www.rwjf.org/en/our-focus-areas/topics/built-environment-and-health.html (accessed August 5, 2020).
13 Hill, D. A neighborhood’s built environment may have numerous effects on its residents’ health. Robert Wood Johnson Foundation. 2014. (accessed August 5, 2020).
14 The Chartis Group. The rural health safety net under pressure: rural hospital vulnerability. 2020. (accessed August 5, 2020).
15 Association of American Medical Colleges. New AAMC report confirms growing physician shortage. 2020. (accessed August 5, 2020).
16 Robert Wood Johnson Foundation and University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps. Measures and Data Sources. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources (accessed August 4, 2020).
17 Magnan, S. Five plus five. NAM Perspectives. Discussion Paper, 2017. doi: 10.31478/201710c.
18 Bibbins-Domingo, K. JAMA. 2019 [published online ahead of print]. doi:10.1001/jama.2019.15603.
19 Graham, G., et al. Health Affairs Blog. 2015. https://www.healthaffairs.org/do/10.1377/hblog20150806.049730/full/ (accessed August 20, 2020)
