Honoring Black History, Healthy Hearts, and Community Initiatives to Address Structural Inequities
By Drs. Janine A. Clayton and Miya Whitaker

Each February the nation celebrates Black History Month, and a few years ago NIH’s theme was “Small Actions, Big Impact: Using Allyship to Enhance Our Culture.” As the director of ORWH, I recognize the importance of creating an organizational culture of inclusion and providing everyone the opportunity to make change. Each of us has the power to choose inclusive actions with our speaking and our behavior. February is also American Heart Month. Cardiovascular disease affects people from all walks of life, all genders, and all ages. It can present differently in women than in men and remains a leading cause of death in women. I encourage all of us to prioritize taking small, heart-healthy actions to make change, such as adding fruits and vegetables to daily meals or taking the stairs rather than the elevator. The National Heart, Lung, and Blood Institute (NHLBI) developed tools to help all of us live a heart-healthy lifestyle. Its website has activities, suggestions, and resources for American Heart Month. I particularly like “28 Days Towards a Healthy Heart.”
Remarkable achievements have occurred, and barriers have been broken, to advance science, health, and health care—globally and locally—to address health disparities. I’m excited to tell you about an NIH-wide effort in which ORWH is partnering with other institutes, centers, and offices to accelerate science and advance health equity.

Community Initiatives to Address Structural Inequities
The Community Partnerships to Advance Science for Society (ComPASS) Program supports community-driven research partnerships that develop ways to intervene at multiple levels—from the personal to the structural—to tackle health disparities in underserved communities. We at ORWH are excited about this program because it expands the approach to health care from an individual-level focus to the wider health context, encompassing sociocultural factors that constrain or promote health, collectively known as social determinants of health (SDOH). The Centers for Disease Control and Prevention has stated that “SDOH have been shown to have a greater influence on health than either genetic factors or access to health care services.” This is why the ComPASS research model employs community-academic partnerships that implement structural interventions, which identify the source of the problem and attempt to change the social, physical, or economic environments that contribute to the presence and persistence of health disparities. For example, one type of structural change could involve creating local, sustainable, healthy food network programs to improve access to and affordability of fresh produce. Another structural change would involve changing policies to restore food-related sovereignty and reduce environmental pollutants. When structural factors change, it becomes possible to affect the health of a larger number of people and improve multiple health outcomes simultaneously.
The ComPASS Program has three components:
- Community-led Health Equity Structural Interventions (CHESIs), through which community organizations and their chosen research partners develop and implement an SDOH project;
- Health Equity Research Hubs, which provide localized technical assistance and scientific support to the CHESIs; and
- ComPASS Coordination Center, which leads program management, coordinates data collection and assessment, and assists with research capacity-building and training.
I want to highlight 2 of the 25 funded CHESIs, one of which directly addresses women’s health and involves ORWH, with a staff member serving as the project scientist.
- The Delta Health Alliance, Inc. (DHA) proposed a Partnership to Optimize Equity in Maternal and Infant Health, which will address maternal and infant morbidity and mortality in five rural, impoverished counties of the Mississippi Delta. In collaboration with local practitioners, social service providers, policy advocates, faith-based communities, and a regional advisory group, DHA will first identify unique structural elements that contribute to maternal and infant health disparities in communities. It will then partner with the Center for Community Research and Evaluation to develop and implement the most appropriate and sustainable structural intervention(s). The work will prioritize addressing structural barriers and policies that contribute to generational cycles of insufficient access to care and high rates of maternal and infant mortality and morbidity.
- Grupo Nexos, Inc. proposed the Puerto Rico Collaborative Advancement of Research, Innovations, Best Practices and Equity for Children, Youth, and Families (PR-CARIBE). Children and youth in Puerto Rico experience the highest economic and social inequality in the United States. PR-CARIBE will intervene in sociocultural factors affecting developmental outcomes in resource-limited children by conducting a needs assessment, developing strategic plans, and then implementing policies to scale-up sustainable strategies that foster equity and wellness across the lifespan.
The ComPASS Program is funded by the NIH Common Fund, which supports high-impact, NIH-wide programs. Common Fund programs are managed by the Office of Strategic Coordination in the NIH Office of the Director.
Black History Month
The theme this year at NIH is Black Excellence in Health and Science. Black History has been about overcoming obstacles and barriers. Although underrepresented in science and medicine, especially in leadership positions, many courageous trailblazing Black women and Black people have existed throughout history, including the first Black female physician, Dr. Rebecca Crumpler, and the first Black female surgeon admitted to the American College of Surgeons, Dr. Helen Dickens. ORWH taps into the wisdom of those who came before us as well as our current voices at NIH in the Pearls of Wisdom video series. This month, I invite you to tune into the wisdom of our featured leader-catalysts, including Keri F. Allen, Caryn Cobb, Yvonne C. Collins, Wendy Wills El-Amin, Gary H. Gibbons, Eve Higginbotham, Leslie Stiff Jones, Michelle Wilson Latting, Vivian Pinn, and Adrienne W. Scott
American Heart Month
Heart disease is the leading cause of death in both men and women in the United States, resulting in one in five deaths among women. However, heart failure can present and progress differently in women. Researchers have now identified many fundamental physiological sex differences, which can lead to differences in risk, in diagnosis, and in treatment. For example, hypertension is more prevalent among people who are Black. In women who are Black, the prevalence was 56.7% compared with approximately 37% for women who are White or Hispanic. Because some still consider women to be at lower risk of cardiovascular disease than men, even when they present with the same measurable risk factors, women must be aware of the facts about heart health. When presenting with symptoms of heart disease, women are less likely than men to have their cardiac risks assessed or to receive guideline-based primary and secondary prevention and are more likely to receive a mental health diagnosis. Further, women who are African American, Hispanic, or Pacific Islander may be more likely to have myocardial infarction with non-obstructive coronary arteries (43% versus 24% for obstructive coronary artery disease).
In 2022, NIH formed a public-private partnership with the U.S. Food and Drug Administration, multiple biopharmaceutical and life sciences companies, and nonprofit organizations to study heart failure that preferentially affects women called heart failure with preserved ejection fraction. It occurs when the left ventricle of the heart is too stiff to refill properly. Current treatments have not been effective for all patients because of clinical variation in this condition. This partnership seeks to understand the subtle phenotypic differences in order to develop more directed and focused therapies.
Heart conditions that develop during pregnancy can pose a significant threat to health for the remainder of the life course. Cardiovascular disease is a common cause of maternal morbidity and mortality, especially in women who are Black. Compared with women who are White and had similar low ejection fraction at diagnosis (ejection fraction is the percentage of blood leaving the ventricle each time it contracts), Black women had more severe left ventricular dysfunction leading to worse outcomes and lower ejection fraction entering the subsequent pregnancy.
NHLBI, ORWH, and others are partnering on the Maternal Health Community Implementation Project (MH-CIP). This initiative supports research coalitions that are embedded in rural communities so that they can develop and test ways to increase the adoption, uptake, and scaling up of evidence-based interventions to improve health before, during, and after pregnancy. Four projects, working in six states (Georgia, North Carolina, South Carolina, New York, Louisiana, and California), include studies of pre-pregnancy counseling, nutrition, and lifestyle counseling during pregnancy; type 2 diabetes prevention; and use of an Outpatient Severe Hypertension Safety Bundle.
NHLBI and ORWH, along with the Eunice Kennedy Shriver National Institute of Child Health and Development and the National Institute of Nursing Research, support the Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone Community Implementation Project (IMPROVE-CIP). Like the MH-CIP, the IMPROVE-CIP focuses on issues leading to maternal illness and death, including mental health, substance use, psychosocial factors, and social and structural determinants of health; however, its work spans broader geographic regions—urban and rural—that have been hit hardest by the maternal health crisis. Chronic exposure to inequities has been linked to cumulative emotional and biological stress affecting heart health in Black and Brown communities. Nevertheless, “when a complex system is far from equilibrium, small islands of coherence…have the capacity to lift the entire system,” according to Nobel Prize–winning chemist Ilya Prigogine. We at ORWH are intent on being an “island of coherence” that lifts the well-being of all women, rippling out to all people.
Community-led Health Equity Structural Intervention (CHESI) Locations
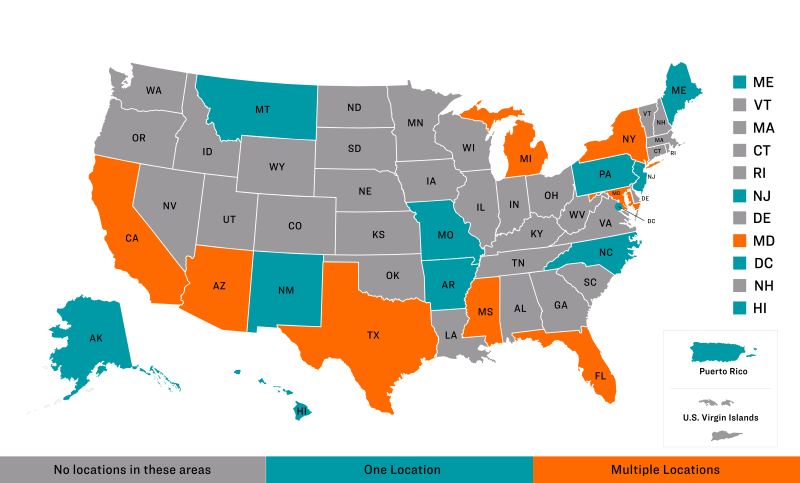
Alabama (AL)
Colorado (CO)
Connecticut (CT)
Delaware (DE)
Georgia (GA)
Idaho (ID)
Illinois (IL)
Indiana (IN)
Iowa (IA)
Kansas (KS)
Kentucky (KY)
Louisiana (LA)
Massachusetts (MA)
Minnesota (MN)
Nebraska (NE)
Nevada (NV)
New Hampshire (NH)
North Dakota (ND)
Ohio (OH)
Oklahoma (OK)
Oregon (OR)
Rhode Island (RI)
South Carolina (SC)
South Dakota (SD)
Tennessee (TN)
Utah (UT)
U.S. Virgin Islands
Vermont (VT)
Virginia (VA)
Washington (WA)
West Virginia (WV)
Wisconsin (WI)
Wyoming (WY)
Alaska (AK)
Arkansas (AR)
District of Columbia (DC)
Hawaii (HI)
Maine (ME)
Missouri (MO)
Montana (MT)
New Jersey (NJ)
New Mexico (NM)
North Carolina (NC)
Pennsylvania (PA)
Puerto Rico (PR)
Arizona (AZ)
California (CA)
Florida (FL)
Maryland (MD)
Michigan (MI)
Mississippi (MS)
New York (NY)
Texas (TX)
