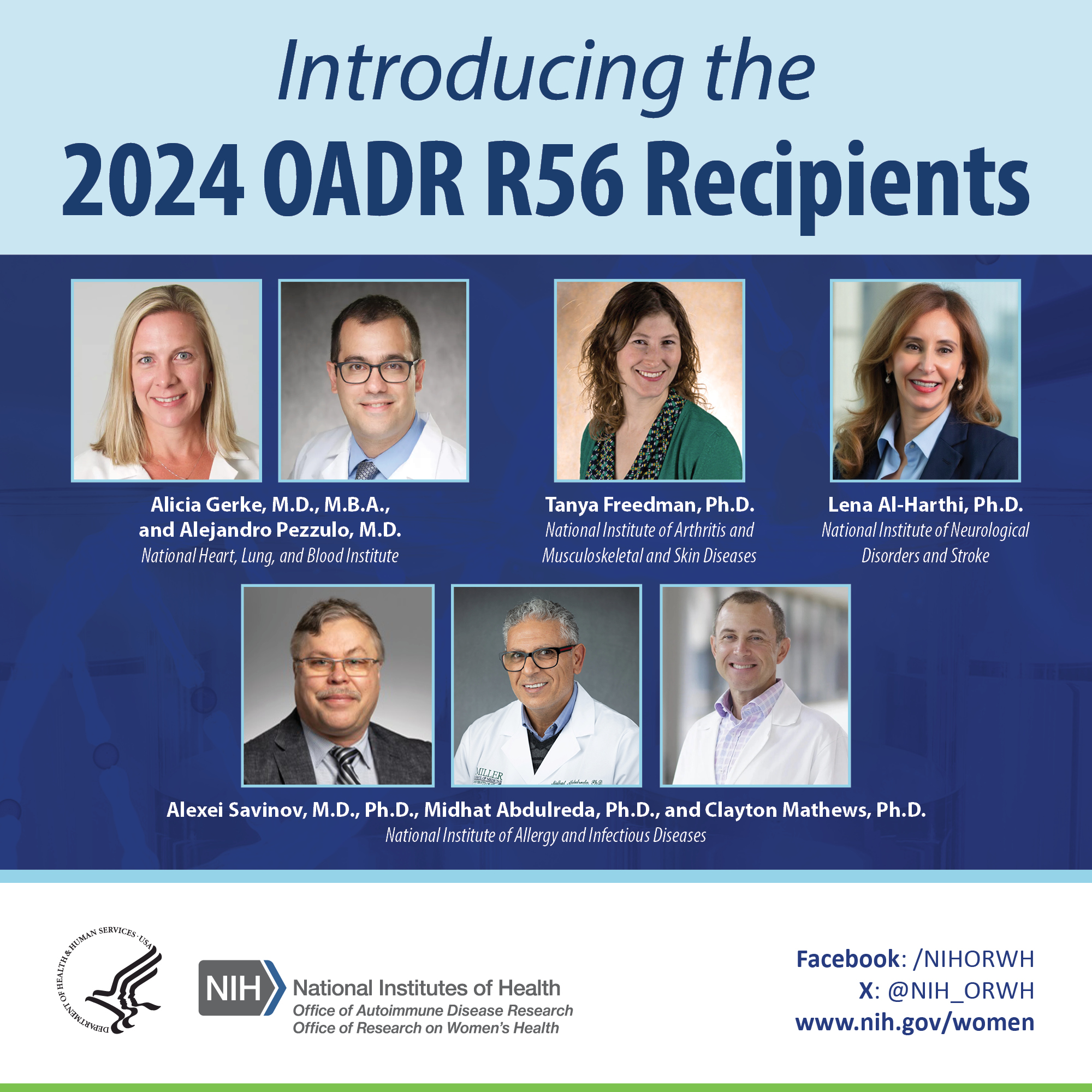
The Office of Autoimmune Disease Research in the Office of Research on Women’s Health (OADR-ORWH) is pleased to introduce the investigators who received the 2024 Office of Autoimmune Disease Research R56 Research Awards. R56 awards support short-term, highly meritorious extramural research that falls just outside the funding limits of participating NIH institutes and centers (ICs). Investigators do not apply for R56 grants. Instead, ICs identify when an R01 application proposes creative and innovative approaches that, if not funded, would represent a missed opportunity to move the field forward. These R01s are then evaluated to determine if they are suitable for conversion to the R56 mechanism. The resulting interim funding allows investigators to complete part of the proposed work with the goal of gathering the data needed to support a future R01 submission of their original idea, effectively avoiding a pause of progress in crucial research areas. The 2024 OADR-ORWH R56 awards, which will support research focused on autoimmune disease topics highly impactful to quality of life and survival, represent individual collaborations between OADR-ORWH and the National Heart, Lung, and Blood Institute (NHLBI), the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), and the National Institute of Neurological Disorders and Stroke (NINDS). Learn more about the awardees and their important work below.
Alicia Gerke, M.D., M.B.A., and Alejandro Pezzulo, M.D., University of Iowa
In the application “The Role of Residential Bioaerosol Exposure in Pulmonary Sarcoidosis,” supported by OADR-ORWH and NHLBI, Alicia Gerke, M.D., M.B.A., and Alejandro Pezzulo, M.D., propose to focus on people with pulmonary sarcoidosis to study the role of household exposure to bacteria and fungi in progression to severe lung disease. This knowledge could guide the development of household environmental remediation strategies for pulmonary sarcoidosis that prevent lung disease progression into dangerous stages that lead to lung transplant or death.
Dr. Gerke is an Associate Professor of internal medicine-pulmonary, critical care and occupational medicine and a practicing pulmonologist at the University of Iowa, with clinical expertise on sarcoidosis and other lung diseases. She obtained her M.D. at the University of South Florida in 2002 followed by residencies in internal medicine at Duke University and the University of Iowa. In 2008, she completed her fellowship on pulmonary disease and critical care medicine at the University of Iowa. Dr. Gerke is the President of the Americas Association of Sarcoidosis and Other Granulomatous Disorders, among other professional affiliations. Her sarcoidosis research focuses on identifying disease mitigating factors, biomarkers, and outcomes measures that truly reflect the clinical experience of people living with sarcoidosis.
Dr. Pezzulo is an associate professor of internal medicine-pulmonary, critical care, and occupational medicine and a practicing pulmonologist at the University of Iowa, with clinical expertise in multiple chronic lung diseases. In 2005, he obtained his M.D. at the Universidad Central de Venezuela, Caracas. From there, he joined the University of Iowa where he completed a postdoctoral fellowship in 2012, a residency on internal medicine in the physician-scientist training program in 2014, and a fellowship on pulmonary disease and critical care medicine in 2017. Soon after, he joined the faculty at the University of Iowa. In his sarcoidosis research, Dr. Pezzulo combines hypothesis-driven and data-driven approaches to study chronic lung diseases, identify predictors of disease progression and optimize treatment in order to avoid severe lung disease.
Alexei Savinov, M.D., Ph.D., Sanford Research and University of South Dakota, Midhat Abdulreda, Ph.D., University of Miami, and Clayton Mathews, Ph.D., University of Florida
In the application “Engineering Human T Regulatory Cells with Chimeric Antigen Receptor Targeting NDTPase3 on the Surface of β Cells for Type 1 Diabetes Control,” supported by OADR-ORWH and NIAID, Alexei Savinov, M.D., Ph.D., Midhat Abdulreda, Ph.D., and Clayton Mathews, Ph.D., propose to create and validate a new regulatory T cell (Treg) therapy for type 1 diabetes (T1D) for future testing in clinical trials. People with T1D have deficiencies in number and function of Tregs, which are an important mechanism for limiting autoimmunity. By developing engineered Tregs with a chimeric antigen receptor (CAR) that recognizes the unique pancreatic beta cell surface antigen NDTPase3, the investigators anticipate that the engineered CAR Tregs will accumulate within the pancreatic islets exerting a local inhibitory effect on self-reactive T effector lymphocytes and preventing further autoimmune damage. This research seeks to improve the functional preservation of pancreatic beta cells and will pave the way for potential future clinical trials of CAR Treg therapy for T1D.
Dr. Savinov is an Associate Scientist at the Sanford Research, Diabetes Group and Associate Professor in the Department of Pediatrics at the Sanford School of Medicine, University of South Dakota. Dr. Savinov obtained his M.D. at the Pavlov’s First Medical Academy in St. Petersburg, Russia, in 1988. In 1993, he earned a Ph.D. in biochemistry from the Institute of Experimental Medicine at the Russian Academy of Medical Sciences. Dr. Savinov completed postdoctoral training in the field of cell biology at the Department of Pharmacology and Experimental Therapeutics in the University of Maryland, Baltimore. He then joined The Jackson Laboratory in Bar Harbor, Maine, where he gained research expertise in immunology. Currently, the Savinov laboratory combines basic and translational science to understand how immune cell signaling in T1D leads to activation of autoimmunity, destruction of insulin-producing beta cells, and manifestation of disease.
Dr. Abdulreda is a Senior Scientist at the Diabetes Research Institute (DRI) and Associate Professor in the Departments of Surgery, Microbiology and Immunology, and Ophthalmology at the University of Miami, Miller School of Medicine. Dr. Abdulreda obtained his Ph.D. in physiology and biophysics in 2007 at the University of Miami. His postdoctoral training at the DRI focused on the immunobiology of T1D and islet transplantation. Later, he continued this research path by joining the faculty at the University of Miami and establishing his laboratory at the DRI. Among other findings, Dr. Abdulreda’s research resulted in the development of a model that uses the eye to measure immune responses against and protection of pancreatic cells, both in the context of autoimmunity and cell transplantation. He is also the Investigational New Drug holder and Principal Investigator on a first-of-its-kind clinical trial (NCT02846571) evaluating the safety of intraocular islet transplantation with localized maintenance immunosuppression via topical application of eye drops in insulin-dependent diabetic patients.
Dr. Mathews is a Professor and Chair, Department of Infectious Disease and Immunology at the University of Florida in Gainesville. Dr. Mathews obtained his Ph.D. from the University of Georgia in 1997 where his studies focused on diabetes and beta cell function. He followed this training by joining The Jackson Laboratory in Bar Harbor, Maine, where he gained postdoctoral expertise in genetics and immunology. His lab at the University of Florida focuses on studying the signaling pathways that lead to beta cell loss and the clinical symptoms in T1D and how these are influenced by genetic and environmental factors.
Tanya Freedman, Ph.D., University of Minnesota
In the application “Functions of LynA and LynB Kinases in Dendritic-Cell Pro-Inflammatory Signaling and Lupus,” supported by OADR-ORWH and NIAMS, Tanya Freedman, Ph.D., proposes to investigate lupus progression and the sex-specific roles of two forms of a protein called Lyn, an enzyme involved in immune modulation and autoimmunity. This research aims to elucidate apparent paradoxes related to Lyn signaling and its contributions to autoimmune disease, which may reveal potential therapeutic targets to suppress lupus progression.
Dr. Freedman is an Associate Professor in the Department of Pharmacology, Center for Immunology, and Masonic Cancer Center at the University of Minnesota. In 2007 she obtained her Ph.D. in molecular and cell biology at the University of California, Berkeley, where she studied the structural biology of a group of proteins (known as Ras-activating proteins) that regulate cell proliferation, inflammation, and other functions. During her postdoctoral work in the laboratory of Arthur Weiss, M.D., Ph.D., at the University of California, San Francisco, Dr. Freedman made important discoveries about the role of LynA in proinflammatory activation, a signaling pathway relevant for autoimmune diseases. Since becoming faculty at the University of Minnesota, her research has focused on multiple pathways that tune responses to inflammatory signaling, in search of strategies that halt the progression of autoimmune disease and cancer.
Lena Al-Harthi, Ph.D., RUSH University Medical Center
In the application “Antibodies in the Neurologic Effects of COVID-19,” supported by OADR-ORWH and NINDS, Lena Al-Harthi, Ph.D., proposes to study aberrant antibodies in the context of COVID-19 disease to understand how they trigger inflammation and autoreactivity. This research aims to elucidate the role of inflammatory antibodies in the acute and chronic neurological manifestations of COVID-19. This work may advance the scientific understanding of both COVID-19 complications that significantly affect quality of life, and other forms of autoimmune encephalitis.
Dr. Al-Harthi is the Vice Dean of Research and a Professor and Chair in the Department of Microbial Pathogens and Immunity at RUSH Medical College. Dr. Al-Harthi earned her Ph.D. in microbiology from The George Washington University. Her dissertation was conducted under the mentorship of Suresh Arya, Ph.D., in the laboratory of Robert Gallo, M.D., co-discoverer of HIV. From there, Dr. Al-Harthi continued postdoctoral training in HIV immunology as a Mark Weiss Fellow of infectious diseases at RUSH University Medical Center, where she joined the faculty in 2000. Her research has focused on defining mechanisms of neurocognitive disturbance associated with chronic viral infections—particularly HIV-associated neurocognitive disorder, which is a collection of thinking, movement, and mood complications experienced by people with HIV. More recently, Dr. Al-Harthi has been applying her vast expertise to the neuroinflammatory complications of HIV to better understand the long-term neurological sequelae of COVID-19.
