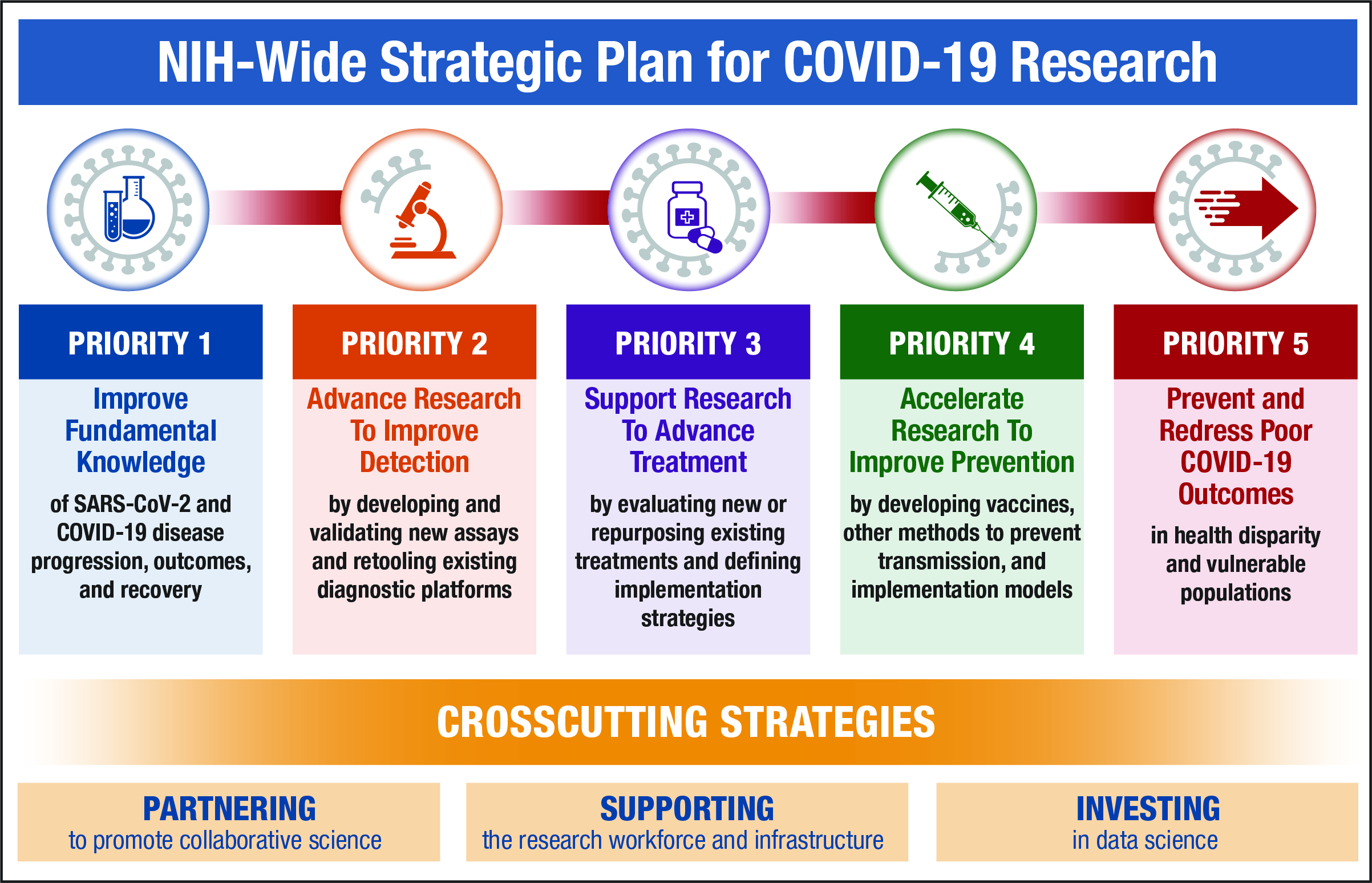
NIH recently released the NIH-Wide Strategic Plan for COVID-19 Research. The strategic plan describes five priorities for accelerating the development of therapeutic interventions, vaccines, and diagnostics:
- Investing in NIH and NIH-funded researchers to increase fundamental and foundational knowledge of SARS-CoV-2 and COVID-19
- Speeding innovation in COVID-19 testing technologies through NIH’s recently launched Rapid Acceleration of Diagnostics (RADx) initiative, which aims to deliver rapid, widely accessible testing strategies to the public
- Participating in public‒private partnerships, such as NIH’s Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) partnership and Federal partnerships such as Operation Warp Speed, to forge groundbreaking approaches that speed identification, development, evaluation, and manufacturing of promising candidate therapeutics and vaccines
- Supporting studies on preventive treatments and behavioral and community prevention practices to identify and implement effective approaches for promoting individual and community safety
- Ensuring that diagnosis, treatment, and prevention options are accessible and available for underserved and vulnerable populations that have been at greatest risk for the most severe threats of the disease
Many of the goals of the NIH-Wide Strategic Plan for COVID-19 Research intersect with ORWH mission areas. ORWH will continue to advance fulfillment of these goals through co-funding and other efforts. These ORWH mission areas include:
- NIH Policies on Inclusion and Sex as a Biological Variable (SABV). NIH’s inclusion policies (i.e., Inclusion Across the Lifespan and Inclusion of Women and Minorities as Subjects in Clinical Research) and SABV policy informed the creation of the strategic plan and will ensure that NIH’s efforts and NIH-funded research will benefit everyone. Studies to examine biological factors that influence individual susceptibility to infection—such as age, sex, gender, genetics, and environment—already are in progress. Researchers also are examining social factors related to COVID-19, such as health disparities based on race and ethnicity, including their influence on biological factors. Also planned are studies of risk factors, complications, and long- and short-term outcomes in older adults, children, and adolescents. In addition, NIH has established a multipronged approach to discover or repurpose promising candidate therapies by using human cell–based and animal models to identify promising therapies that might interfere with the production of the virus or the ability of the virus to infect cells; this research will proceed according to the SABV policy.
- Understudied, Underrepresented, and Underreported (U3) Interdisciplinary Research. NIH recognizes the disproportionate impact of COVID-19 on health disparity, vulnerable, and U3 populations and is striving to mitigate it by identifying the underlying factors and barriers that contribute to the staggering losses in these communities. Inclusion of these populations in clinical trials for diagnostics and interventions will be a critical part of NIH’s pandemic response, as will exploring communication strategies and ways to improve access to care and interventions for at-risk populations. In particular, one of the key components of the RADx initiative, RADx Underserved Populations (RADx-UP), will leverage existing community partnerships to build community-engaged demonstration projects focused on identifying effective implementation strategies to enable and enhance testing for underserved and vulnerable populations.
- Maternal Health. The strategic plan articulates how NIH will examine and address COVID-19 as it relates to maternal health and pregnancy outcomes. Ongoing and future studies will include consideration of COVID-19 and maternal morbidity, pregnancy-related alterations to the immune system, preterm birth, infant health, prenatal and postnatal care, rate of cesarean section delivery, possible mother-to-fetus transmission, possible mother-to-child transmission at birth, and possible transmission via breastfeeding. Independent of COVID-19, women in the United States from underserved populations face substantially higher rates of pregnancy-related complications (e.g., severe maternal morbidity) and pregnancy-related death compared with non-Hispanic White women. As such, NIH will leverage existing research on maternal morbidity and mortality to investigate questions related to pregnancy and COVID-19 among different populations.
You can read the NIH-Wide Strategic Plan for COVID-19 Research and learn more about how the framework aims to mobilize the biomedical research response to the pandemic here.