NIH Women's Health Roundtable: Maternal Mental Health Research
Date and Time
– September 16, 2024, 4:30 PM EDTVirtual Only.

Elevating Women’s Voices to Improve Maternal Mental Health is the third roundtable of the NIH Women’s Health Roundtable Series, which focuses on important women’s health topics, such as maternal mental health, as part of the White House Women’s Health Research Initiative. This series was developed as a recommended action in response to the Presidential Memorandum to bring attention to priority topics within the Department of Health and Human Services (HHS) and to disseminate information on federally supported research areas.
The roundtable is also featured in the National Institute of Mental Health’s (NIMH) Office of Disparities Research and Workforce Diversity Webinar Series, which focuses on mental health equity research topics. The event is co-hosted by NIH’s Office of Research on Women’s Health and NIMH.
The goals of this roundtable are to:
- Spotlight high priority research areas related to women's mental health during pregnancy and the postpartum period, up to one year following childbirth.
- Share information on how NIMH-supported research advances the development of and access to screening, diagnostics, and preventive and treatment interventions to improve women’s mental health during the perinatal period.
- Explain how maternal mental health research can reduce the burden of mental illnesses that contribute to maternal morbidity and mortality.
- Identify and explore gaps in areas critical to women’s research outlined within the Executive Order on Advancing Women's Health Research and Innovation (EO 14120) and the 2024-2028 NIH-Wide Strategic Plan for Research on the Health of Women.
Registration:
This webinar is free, but registration is required.
Sponsored by:
NIMH’s Office for Disparities Research and Workforce Diversity and NIH’s Office of Research on Women’s Health
Contact:
For questions, please contact Tamara Lewis Johnson.
 | Lyndsay Ammon Avalos, Ph.D., M.P.H. Research Scientist III Division of Research Kaiser Permanente Northern California Dr. Avalos is a senior research scientist and director of the Postdoctoral Translational Research Fellowship at the Division of Research at Kaiser Permanente Northern California and an associate professor at the Bernard J. Tyson Kaiser Permanente School of Medicine. Her research is primarily focused on informing and developing innovative interventions to improve the mental health and well-being of pregnant individuals, new parents, and their children. More specifically, her research in maternal mental health and substance use includes epidemiologic studies on maternal and child health outcomes as well as disparities in perinatal mental health, addressing prevention, evaluating screening and treatment, conducting randomized controlled trials to test interventions, and identifying barriers and avenues for intervention implementation into health care delivery. Her research also includes pharmacoepidemiologic studies of the effects of prenatal depression and its treatment on neonatal and neurodevelopmental outcomes in the offspring. Dr. Avalos has received funding for research and training from NIMH, the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and Kaiser Permanente. |
 | Christina Borba, Ph.D., M.P.H. Director, Office of Disparities Research and Workforce Diversity (ODWD) National Institute of Mental Health (NIMH) Dr. Borba is the director of ODWD at NIMH. She leads the development and implementation of scientific policies and research initiatives aimed at reducing mental health disparities and advancing equity in mental health interventions, services, and outcomes. Her work also focuses on increasing workforce diversity and scientific attention to mental health disparities experienced by women and people living in rural areas. Her career spans more than 20 years and includes experience informing and developing evidence-based interventions to mitigate disparities in mental health among marginalized populations. Her most recent research focused on psychotic disorders and cultural psychiatry in low-resourced settings in the United States and abroad, women’s mental health, and gender differences in care. |
 | Nicole Christian-Brathwaite, M.D. CEO and Founder, Well Minds Psychiatry and Consulting Adult, Child, and Adolescent Psychiatrist Dr. Christian-Brathwaite is a nationally recognized board-certified adult, child, and adolescent psychiatrist. She is the CEO and Founder of Well Minds Psychiatry and Consulting Company. Dr. Christian-Brathwaite has expertise in perinatal and postpartum mental health, trauma-informed care, telepsychiatry, mental health in communities of color, school psychiatry, implicit bias, and racism in mental health. She has extensive clinical experience with adults, children, adolescents, and transitional and college-aged youth. She was selected as a member of the inaugural class of the Women’s Wellness Through Equity and Leadership program, sponsored by the American Psychiatric Association and the American Physician’s Foundation. She has given lectures throughout the country on topics such as “Adverse Childhood Experiences in the School Environment,” “Prioritizing Self Care,” and “Postpartum Depression in Women of Color.” Dr. Christian-Brathwaite continues to endeavor to provide excellent clinical care and teaching, while committing a significant amount of time to serving the community at large. She is frequently asked to give talks in the community, on the radio, and at conferences about resiliency, stress management, preventive mental health care, and mental illness. |
 | Samantha Meltzer-Brody, M.D., M.P.H. Assad Meymandi Distinguished Professor Chair, Department of Psychiatry Director, Center for Women’s Mood Disorders University of North Carolina (UNC), Chapel Hill Dr. Meltzer-Brody is the Assad Meymandi Distinguished Professor and chair of the Department of Psychiatry at UNC Chapel Hill. She also directs the UNC Center for Women’s Mood Disorders. She is a passionate advocate for innovation and transformation of mental health care. She has also served in leadership roles in physician and health care worker mental health and wellbeing in the School of Medicine and UNC Health. Dr. Meltzer-Brody is an internationally recognized physician-scientist in perinatal depression. Her research investigates the epidemiologic and biological predictors of perinatal depression and innovative treatment approaches (pharmacologic and psychotherapeutic), which have taken her across the globe including to sub-Saharan Africa. She had led the MOMS GENES study—the largest global genetic study of postpartum depression using app-based tools. She also served as the academic principal investigator for the novel psychopharmacologic clinical trials developing the first U.S. Food and Drug Administration approved medication for postpartum depression, brexanolone, and served as an investigator for the newly approved oral drug, zuranolone, for postpartum depression. She was named to the 2022 Forbes list of “16 Healthcare Innovators You Should Know,” the 2021 Forbes The Visionary List: Women Over 50 Shaping The Future Of Science, Technology And Art, and the Forbes list of “Women Over 50 Working To Improve Our Collective Mental Health.” She was also ranked in 2021 by Expertscape, as the number one expert in the world for postpartum depression. |
 | Dana Meaney-Delman, M.D. Chief, Infant Outcomes Monitoring, Research, and Prevention Branch U.S. Centers for Disease Control and Prevention (CDC) Dr. Meaney-Delman is the chief of the Infant Outcomes Monitoring, Research and Prevention Branch in the National Center for Birth Defects and Developmental Disabilities at CDC. She was the co-lead for the Data, Research, and Quality Improvement Subcommittee of the Department of Health and Human Services Task Force on Maternal Mental Health. She founded the Emerging Threats to Mothers and Babies initiative, which identifies and responds to emerging and reemerging infectious disease threats. Previously, she served as senior medical advisor for preparedness in the National Center for Emerging and Zoonotic Infectious Diseases at CDC, where she worked to prepare the nation against infectious threats, developing clinical guidelines on anthrax, smallpox, Ebola, botulism, plague, and Zika virus. She has authored more than 70 peer-reviewed articles primarily focused on infectious diseases. Dr. Meaney-Delman practices general OB/GYN as an adjunct assistant professor at Emory University. She holds board certification in obstetrics and gynecology. |
 | Sheehan D. Fisher, Ph.D. Associate Professor, Department of Psychiatry and Behavioral Sciences Northwestern University, Feinberg School of Medicine Dr. Fisher is an associate professor and perinatal clinical psychologist at Northwestern University, Feinberg School of Medicine, and associate dean for diversity and inclusion at The Graduate School at Northwestern University. His research career focuses on the effects of perinatal and subsequent parental mental health on infant/child health outcomes. His aim is to reconceptualize parental mental health research to integrally involve both birthing and non-birthing parents to differentiate parents’ impact on child mental and developmental health. Dr. Fisher’s research dovetails with his perinatal mental health clinical practice where he utilizes behavioral therapies to support parents’ transition into the perinatal period and beyond. Ultimately, his goal is to optimize the health and effectiveness of the parental team to positively influence the child and family health trajectory starting during pregnancy. |
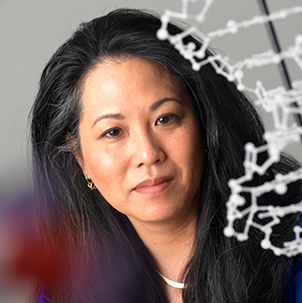
 | Ai Kubo, Ph.D., M.P.H. Research Scientist and Epidemiologist Division of Research (DOR) Kaiser Permanente Northern California Dr. Kubo is a research scientist and epidemiologist in the DOR at Kaiser Permanente Northern California. She received her doctorate in cancer epidemiology at the Columbia Mailman School of Public Health in 2007 and has been conducting research at the DOR since 2005. Dr. Kubo’s research portfolio reflects her strong interest in life course epidemiology and health disparities. She has extensive experience examining perinatal biological and psychosocial determinants of adolescent health including early puberty and mental health as well as conducting mindfulness-based intervention studies targeting pregnant women. Currently, she is the principal investigator of two NIH-funded R01s: “Sex and Race/Ethnicity-specific Multilevel Factors Influencing Pubertal Trajectories: A Population-based Study” and “mHealth Mindfulness Intervention for Pregnant Black and Latina Women at Risk of Postpartum Depression.” |
 | Catherine Monk, Ph.D. Diana Vagelos Professor of Women’s Mental Health Chief, Division of Women’s Mental Health, Department of Obstetrics and Gynecology Columbia University Dr. Monk is the Diana Vagelos Professor of Women’s Mental Health and chief of the Division of Women’s Mental Health in the Department of Obstetrics & Gynecology (OB/GYN) and professor of medical psychology in the Department of Psychiatry at Columbia University Vagelos College of Physicians and Surgeons. She is a research scientist VI at the New York State Psychiatric Institute. Dr. Monk directs Women’s Mental Health at OB/GYN, an integrated service within OB/GYN, and conducts perinatal mental health research with a two-generation focus. Her research has been continuously funded by NIH since her NIH career development award in 2000 as well as by numerous foundations, including the Bezos Family Foundation, the Robin Hood Foundation, March of Dimes, and the Brain and Behavior Research Foundation. |
 | Wanjikũ F.M. Njoroge, M.D. Associate Professor, Department of Psychiatry University of Pennsylvania, Perelman School of Medicine Associate Chair of Diversity, Equity, and Inclusion and Accessibility (DEIA), Department of Child and Adolescent Psychiatry and Behavioral Sciences Medical Director, Young Child Clinic Faculty, PolicyLab Children’s Hospital of Philadelphia (CHOP) Dr. Njoroge is an associate professor of psychiatry at the University of Pennsylvania Perelman School of Medicine, associate chair of DEIA for the Department of Child and Adolescent Psychiatry and Behavioral Sciences at CHOP, faculty member at PolicyLab, and medical director of the Young Child Clinic at CHOP. She is a practicing infant/preschool psychiatrist. Dr. Njoroge’s research areas of focus have been on health equity, diversity, and inclusion with a focus on early childhood development and parenting practices. Her core areas of focus have been on prevention, promotion, and early intervention. Her recent work has measured the impact of the pandemic on the mental health and wellbeing of peripartum women and their developing children. She is a standing member of the NIMH section on Psychosocial Development, Risk, and Prevention. She is also a distinguished fellow in the American Academy of Child and Adolescent Psychiatry. |
 | Mary Shaw-Ridley, Ph.D., M.Ed., MCHES Chair, Department of Behavioral and Environmental Health Principal Investigator, Delta Mississippi IMPROVE Center of Excellence Jackson State University (JSU) Dr. Shaw-Ridley currently serves as department chair and professor in the Department of Behavioral and Environmental Health in the College of Health Sciences at JSU, a historically Black college/university. She is the lead program investigator for the JSU-Mississippi Delta Center of Excellence in Maternal Health, funded by the NIH/NICHD IMPROVE Centers of Excellence initiative. She has previously held academic appointments in the Department of Health Promotion and Disease Prevention; Robert Stempel College of Public Health & Social Work at Florida International University, Miami; Texas A&M University, College Station; Indiana University, Bloomington; and Texas Woman’s University, Denton. For several years, Dr. Shaw served as the deputy director of the Social and Health Research Center in San Antonio, Texas, under the direction of Roberto Trevino, M.D., an internist focused on early interventions to reduce childhood obesity among Hispanic and Black children. |
 | Nima Sheth M.D., M.P.H. Associate Administrator for Women’s Services Chair, Advisory Committee for Women’s Services Senior Medical Advisor Substance Abuse and Mental Health Services Administration (SAMHSA) Dr. Sheth is a psychiatrist and the senior medical advisor at SAMHSA’s Center for Mental Health Services, the associate administrator for Women’s Services, and chair of the Advisory Committee for Women’s Services. Dr. Sheth is also the SAMHSA point of contact on the new maternal mental health task force. In addition to leading women’s mental health issues at the agency, Dr. Sheth also specializes in refugee and migrant mental health, implementation science, diversity, equity, inclusion, and accessibility, and the behavioral health workforce and leads the center’s technical assistance efforts. Dr. Sheth also specializes in trauma, serving as psychiatric consultant for various community clinics and leading various trauma initiatives across organizations—both nationally and internationally. She has served as a psychiatric consultant to the World Health Organization and has worked in several international projects, advising on increasing mental health capacity, improving the quality of mental health services, strengthening referral networks, and coordinating collaborative and integrative care. |
 | Melissa Simon, M.D., M.P.H. Vice Chair for Research, Department of Obstetrics and Gynecology Director, Institute for Public Health and Medicine Center for Health Equity Transformation George H. Gardner Professor of Clinical Gynecology Professor of Obstetrics and Gynecology, Preventive Medicine, and Medical Social Sciences Northwestern University Dr. Simon is the George H. Gardner Professor of Clinical Gynecology and vice chair for research in the Department of Obstetrics and Gynecology at the Northwestern Feinberg School of Medicine. Her primary research interests are aimed at promoting health equity and eliminating health disparities among low-income, medically underserved women across the lifespan. Integrating health services research with social epidemiologic models, Dr. Simon’s research focuses on interventions (such as patient navigation and community health outreach workers) that aim to reduce and eliminate such disparities. Within this context, Dr. Simon prefers to leverage culture and community to achieve these goals and thereby integrates community-based participatory research framework into her work. She also has a strong portfolio of workforce development programs including the world’s first health care pipeline development free open online course, “Career 911: Your Future Job in Medicine and Healthcare” on the Coursera platform. She is the founding director of the Center for Health Equity Transformation and the Chicago Cancer Health Equity Collaborative. She is a former member of the U.S. Preventive Services Task Force. She is a member of the National Academy of Medicine (NAM) and the Association of American Physicians. She currently is a member of the NAM Board on Population Health and Public Health Practice and the Roundtable for the Promotion of Health Equity. She also serves as an Advisory Committee member to the NIH Office of Research on Women’s Health. |
 | Vivian Ota Wang, Ph.D. Deputy Director, ORWH National Institutes of Health (NIH) Dr. Ota Wang is the deputy director of ORWH at NIH. She is a psychologist, geneticist, and genetic counselor. Dr. Ota Wang’s domestic and global experiences in research, education, policy, and ethics span biomedical, psychological, genomic, nanoscale, and data sciences. She currently applies her expertise in racial identity, community engagement, and ethics to scientific leadership and oversight of women’s health research as the ORWH deputy director. Previously, she was the inaugural policy, ethics, and COVID lead at the Office of Data Science Strategy where she established the NIH Rapid Acceleration of Diagnostics (RADx) Data Repository, one of the largest NIH COVID-19 databases that accelerated COVID-19 testing in underserved populations. She also envisioned and spearheaded the RADx Tribal Data Repository, the first NIH sovereignty-based research data repository. Prior to public service, she was a genetic counselor at the University of Colorado and then held tenure-track faculty positions at Rutgers University, Arizona State University, and Vanderbilt University where her research focused on racial identity, multicultural competencies, and research participant protection related to research ethics, program development and evaluation, and community engagement. Her clinical expertise is in congenital and acquired disabilities, traumatic brain injury, and bereavement. Her accomplishments are recognized by university, professional, and government awards. |
 | Kara Zivin, Ph.D., M.S., M.A., M.F.A. Marica A. Valenstein Collegiate Professor of Psychiatry Professor, Health Management and Policy Research Career Scientist, Center for Clinical Management University of Michigan Dr. Zivin is the Marcia A. Valenstein Collegiate Professor of Psychiatry, professor of obstetrics and gynecology and of health management and policy at the University of Michigan, research career scientist at the Veterans Affairs Ann Arbor Center for Clinical Management Research, and senior health researcher at Mathematica. Dr. Zivin is a health services and policy researcher who uses social science and public health tools to improve health and functional outcomes for vulnerable populations with mental health and substance use disorders (behavioral health conditions), including pregnant and postpartum women, Veterans, and older adults. She conducts large, mixed-methods research studies and evaluations assessing the intended and unintended consequences of health policies and health system interventions. Dr. Zivin aims to increase public awareness about and influence policy addressing behavioral health conditions by combining research expertise (data) and personal narrative (story). She completed her doctorate and master of science degree at Harvard University, her master of arts and bachelor’s degree at Johns Hopkins University, and her master of fine arts degree at Vermont College of Fine Arts. |
| Time | Agenda |
|---|---|
| 12:00 p.m. – 12:05 p.m. | Introductory Remarks
|
| 12:05 p.m. – 12:20 p.m. | Advancing Women's Mental Health Research
|
| 12:20 p.m. – 12:50 p.m. | From Biology to Breakthrough: The Story of Brexanolone and Zuranolone
|
| 12:50 p.m. – 1:00 p.m. | Questions and Answers |
| 1:00 p.m. – 2:20 p.m. | Session 1: Clinical Perspectives on Maternal Mental Health Research2Gen Perspective on Maternal Mental Health: Prevention & Intervention
mHealth Mindfulness Based intervention for Pregnant Black and Latina Women at Risk for Postpartum Depression
Prevention of Perinatal Depression in Birthing People with a History of Adverse Childhood Experience: A Type 2 Hybrid Effectiveness Trial
Maternal Mental Health Research and the Value of Lived Experience
|
| 2:20 p.m. – 2:35 p.m. | Roundtable Discussion for Session 1 |
| 2:35 p.m. – 2:45 p.m. | Break |
| 2:45 p.m. – 4:05 p.m. | Session 2: Innovative Models of Maternal Mental Health CareAdvancing Maternal Mental Health Care in Rural Mississippi
Investigating Maternal Mental Health and Child Mental Health Experiences of the Syndemic of COVID and Underlying Systemic Conditions
Disparities in Utilization and Delivery Outcomes for Women with Perinatal Mood and Anxiety Disorders: A Groundwork for State Policymaking and Reflections on Lived Experience
Highlights of the National Strategy to Improve Maternal Mental Health Care
|
| 4:00 p.m. – 4:15 p.m. | Roundtable Discussion for Session 2 |
| 4:15 p.m. – 4:25 p.m. | Discussant’s Remarks
|
| 4:25 p.m. – 4:30 p.m. | Closing Remarks
|
