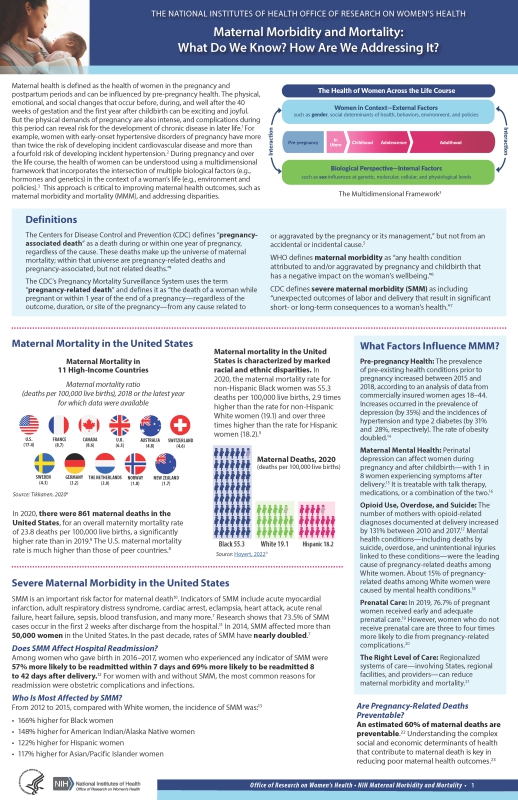
Approximately 700 women die in the U.S. each year because of pregnancy or delivery complications, but an estimated 50% of these are preventable. [1] Despite spending more than any other country on maternity care, the U.S. has one of the highest maternal mortality rates in the developed world. In addition, there are extreme racial and ethnic disparities in rates of pregnancy-related death—defined as the death of a woman while pregnant or within 1 year of the end of pregnancy from any cause related to or aggravated by the pregnancy. [2] Research shows that between 2007 and 2016, Black and American Indian/Alaskan Native women had higher pregnancy-related mortality ratios (PRMRs) than White and Hispanic women. [3] Moreover, Black women have the highest PRMR, regardless of factors such as age, level of education, geographic location, income or higher socioeconomic status. In addition to this alarming finding, overall pregnancy-related mortality is increasing, and the scientific community is still unclear as to why this is occurring.
The World Health Organization defines maternal morbidity as any health condition attributed to and/or aggravated by pregnancy and childbirth that has negative outcomes to the woman’s well-being. [4] As with maternal mortality, maternal morbidity has also seen increasing numbers. Excluding blood transfusions, the rate of severe maternal morbidity (SMM) increased by approximately 20% from 1993-2014 in the U.S. [5] Incorporating frameworks such as the social–ecological model [6] and the multidimensional framework of the health of women across the life course [7] in maternal health research may help us to better understand the factors affecting women from preconception to pregnancy to postpartum periods.
The Life Course Perspective
The 2019–2023 Trans-NIH Strategic Plan for Women’s Health Research is grounded in three guiding principles that emphasize the importance of (1) considering the complex interactions of multiple factors that influence the health of women, (2) including different NIH-designated U.S. health disparity populations (i.e., Blacks/African Americans, Hispanics/Latinos, American Indians/Alaska Natives, Asian Americans, Native Hawaiians and other Pacific Islanders, socioeconomically disadvantaged populations, underserved rural populations, and sexual and gender minorities) in research, and (3) engaging diverse perspectives in the biomedical research enterprise. These guiding principles are based on the idea that the health of women extends beyond reproductive health to encompass a broad spectrum of diseases and conditions experienced by women and recognize that these diseases and conditions are influenced by such factors as sex, race, ethnicity, and age. Those factors interact with social determinants―such as gender, behavior, environment, and policies―across a woman’s life course to influence her health. All of these factors further interact with a woman’s unique biological characteristics at the genetic, molecular, cellular, and physiological levels to determine her health, longevity, and disease and disability outcomes.
The aim of this web portal is to be a hub that provides resources that serve as an educational foundation for researchers, clinicians and the public, to address the critical maternal morbidity and mortality public health issue. For a comprehensive overview of recent scientific research and evidence-based practices relating to MMM, please click the links below to access the ORWH-developed MMM fact sheet and video.
[1] Centers for Disease Control and Prevention. (2019). Pregnancy-related deaths. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-relatedmortality.htm
[2] Centers for Disease Control and Prevention. (2020). Pregnancy mortality surveillance system. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm
[3] Centers for Disease Control and Prevention. (2020). Infographic: racial/ethnic disparities in pregnancy-related deaths — United States, 2007–2016. https://www.cdc.gov/reproductivehealth/maternal-mortality/disparities-pregnancy-related-deaths/infographic.html
[4] Firoz, T. et al. (2013). Bulletin of the World Health Organization. PMID: 24115804.
[5] Centers for Disease Control and Prevention. (2021). Severe Maternal Morbidity in the United States. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
[6] Centers for Disease Control and Prevention. (2021). The social-ecological model: a framework for prevention. https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html
[7] Schweinhart, A., & Clayton, J. A. (2018). International Journal of Environmental Research and Public Health. PMID: 30134570.