Understanding Influences of Sex and Gender in Health and Disease
To learn about the terms “sex” and “gender” visit our page What are Sex & Gender?
Understanding sex and gender is critical to understanding health and to diagnosing and treating disease and illness. Disparities in the prevalence and severity of several conditions point to the need for further research in this area. For example:
- Women are nearly twice as likely as men to be diagnosed with depression. [1]
- Women and men have heart attacks at similar rates, but women are more likely to die as a result. [2]
- Women make up about 78% of patients with autoimmune diseases. [3]
- Women are more likely to have chronic pain than men, but women are less likely to receive treatment. [4]
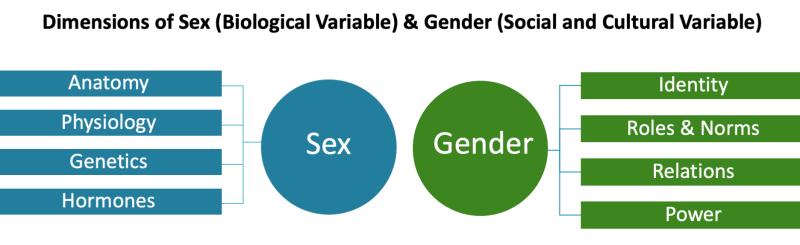
To better understand and address these gaps, it is important to consider how both sex and gender influence these disparities. It is also important to understand that sex and gender are interconnected but distinct concepts, and that each affect health as both independent and interactive factors. The below graphic presents a few examples of sex and gender influences across various areas of health and disease to illustrate the distinction between sex and gender and highlight the importance of understanding them as factors in health and disease. Please note that each example presented below is just one of many possible examples for each area.
One example of how sex influences mental health is that the sex hormones estrogen and progesterone play a role in increasing the activity of key signaling molecules (including dopamine and serotonin) that affect mood. Variations in these sex hormones likely contribute to differences observed between male and female incidence rates of depression, as well as responses to treatment.
LeGates et al., 2019. PMID: 30082889
There are many ways in which gender influences mental health. For example, dominant norms of masculinity—such as self-reliance and toughness—have been shown to negatively influence boys’ and men’s willingness to seek mental treatment. Gender-based violence (power, relations) is associated with an increase in post-traumatic stress, anxiety, and depressive disorders in women.
Riecher-Rössler, 2017. PMID: 27856397
Milner et al., 2019. PMID: 31690213
Because of sex differences in physiology and anatomy, consumption of alcohol leads to greater blood alcohol concentrations and intoxication in females compared with males. The male metabolism of alcohol is more rapid than the female metabolism of alcohol because on average, females have less total body water than males, which affects the distribution of alcohol after absorption.
McHugh et al., 2018. PMID: 29174306
Gender relations—particularly in intimate partnerships—have been shown to influence substance use. For example, many women who begin using injection drugs have been influenced by a male partner. Gendered power dynamics can also make it difficult for women to leave unsafe relationships with partners who use drugs or drink excessively.
Meyers et al., 2020. PMID: 31625809
Wechsberg et al., 2013. PMID: 23927691
The sex hormone estrogen plays a protective role in female cardiovascular function by promoting vasodilation (relaxation of blood vessels) and lowering blood pressure. After menopause, when the amount of circulating estrogen declines, the risk of cardiovascular disease increases in the female population and becomes similar to that seen among males.
Ji et al., 2021. PMID: 33587655
El Khoudary et al., 2020. PMID 33251828
Many women experience a heightened awareness of potential physical and sexual threats, including street harassment and violence. These threats create barriers to women’s participation in physical activity, which is important for lowering cardiovascular risk. For example, women are less likely than men to exercise in public or ride a bike through a city.
O’Neil et al., 2018. PMID: 29459471
The female immune system is generally more robust than the male system, with higher levels of circulating antibodies and greater cytokine release in response to infection. This difference in immune function, as well as genetic factors, contributes to the disproportionate prevalence of autoimmune diseases in females.
Billi et al., 2019. PMID: 30394940
Gender norms related to femininity—including the perception that women are more emotional than men—have been shown to contribute to frequent misdiagnosis of autoimmune symptoms. For example, systemic lupus erythematosus (SLE) is often misdiagnosed as hypochondria or anxiety in women, leading to delays in diagnosis and treatment.
Sloan et al., 2020. PMID: 32373774
Pain processing differs within male and female nervous systems. For example, the sex hormone testosterone, which is present in higher levels in males, has a protective function against pain. In addition, genetic factors may contribute to differences in pain receptors that influence pain sensitivity. These sex differences affect the efficacy of treatments for pain, which are often less effective for female patients.
Bartley & Fillingim, 2013. PMID: 23794645
Farkouh et al., 2021. PMID: 33916167
Gender roles and norms have been shown to affect the diagnosis, treatment, and experience of pain in many ways. For example, women reporting their symptoms may be dismissed as “hysterical” or “emotional,” leading to inadequate treatment for pain; men may be discouraged from seeking medical treatment based on gender norms of masculinity that emphasize toughness.
Samulowitz et al., 2018. PMID 29682130
Access to neighborhood green spaces is a vital component of the built environment. Emerging research suggests that higher neighborhood greenness in areas with low levels of airborne particulate matter is correlated with higher numbers of ovarian follicles (anatomy and physiology) and therefore a slower rate of female reproductive aging.
Hood et al., 2021. PMID: 33905704
Gender norms and structural sexism (power) contribute to occupational segregation of women in service professions, which influences environmental exposures. For example, most workers in nail salons are women (often low-income and immigrant women), and they are disproportionately exposed to endocrine-disputing phthalates in the workplace.
Varshavsky et al., 2020. PMID: 31906553
Chronic exposure to sexual abuse has been found to be associated with an increase in inflammation and impaired wound healing in the female genital tract (anatomy and hormones). The resultant female-specific immune dysregulation can result in greater susceptibility to HIV infection.
Ghosh et al., 2018. PMID: 29894487
Derry et al., 2021. PMID: 34589822
Women experience greater rates of severe physical and/or sexual violence perpetrated by an intimate partner than men, a disparity that is influenced heavily by gender roles, gender norms, and gendered power dynamics. In addition, structural and community-level gendered power dynamics often converge to discourage women from reporting abuse.
CDC, “Preventing Intimate Partner Violence”
Decker et al., 2019. PMID: 31214974
Anatomical differences contribute to a higher prevalence of bladder infections in female patients. Because the female urethra is shorter than that of the male, bacteria have less distance to travel to reach and infect the bladder. In addition, the opening to the female urethra is closer to the rectum, a source of many bacteria that commonly cause bladder infections.
Social and cultural stigma around menstruation is one example of how gender norms can impact health and wellbeing. For example, stigma around menstrual disorders and dismissal of women’s pain as emotional rather than physical have been associated with delayed diagnosis of endometriosis (a menstrual disorder that affects roughly 10% of reproductive-age women) for as long as 11 years from the onset of symptoms, postponing treatment and the alleviation of symptoms.
Sims et al., 2021. PMID: 34360501
Differences between male and female musculoskeletal systems can influence a person’s risk of certain types of injuries. For example, differences in male and female knee and hip anatomy include leg muscle strength and tendon and ligament laxity. These anatomic differences are associated with higher risk of anterior cruciate ligament (ACL) injuries for girls and women.
Lin et al., 2018. PMID: 29550413
Musculoskeletal health can be influenced by cultural expectations of gender expression and norms of femininity. Women are often encouraged or required to wear and walk in high-heeled shoes, which contributes to the increased risk for women of developing osteoarthritis later in life because walking in high heels puts excess stress on knee joints.
Titchenal et al., 2015. PMID: 25532875
Because of differences in anatomy, some cancers are sex-specific. For example, prostate cancer only affects males and ovarian cancer only affects females. In addition, sex differences in the metabolism of chemotherapy drugs influence the severity of side effects—such as significant decreases in white blood cell counts, which more commonly occur among female patients.
Siegel et al., 2022. PMID: 35020204
A cancer diagnosis is one of the most common medical conditions that require adult caregiving. Because of gender roles and norms, women provide most of the paid and unpaid acts of caregiving. Women who are caregivers of a spouse with cancer generally experience higher levels of stress, depression, and anxiety compared with men.
Ketcher et al., 2020. PMID: 31845168
A note on terminology:
“Male” and “female” refer to sex assigned at birth. In addition, while we use the terms “male” and “female” for the purposes of this discussion, we recognize that sex is not a binary construct and variations in sex characteristics do occur. These variations are also called intersex conditions. For more information, visit the website of NIH’s Sexual & Gender Minority Research Office.
[1] Mayo Clinic. (n.d.). Depression in women: Understanding the gender gap. Retrieved January 18, 2023, from https://www.mayoclinic.org/diseases-conditions/depression/in-depth/depression/art-20047725
[2] American Heart Association. (2020, November 30). Women found to be at higher risk for heart failure and heart attack death than men. https://newsroom.heart.org/news/women-found-to-be-at-higher-risk-for-heart-failure-and-heart-attack-death-than-men
[3] Fairweather, D., & Rose, N. R. (2004). Women and autoimmune diseases. Emerging Infectious Diseases, 10(11), 2005–2011. https://doi.org/10.3201/eid1011.040367
[4] International Association for the Study of Pain. (n.d.). Female pain issues. Retrieved January 19, 2023, from https://www.iasp-pain.org/advocacy/global-year/pain-in-women/